The intraoperative fluorescence imaging industry size is projected to be worth USD 758.7 million in 2025. The industry is poised to reach a valuation of USD 2.225 billion by 2035, reflecting a CAGR of 11.9% during the upcoming decade.
The intraoperative fluorescence imaging industry saw tremendous growth in 2024. This growth was fueled by technology, particularly the combination of near-infrared fluorescence (NIRF) imaging and artificial intelligence (AI), which improved real-time visualization during surgery and accuracy.
The increasing incidence of chronic diseases, including cancer and cardiovascular diseases, made it imperative to have sophisticated imaging technologies for precise interventions. The larger number of healthcare personnel becoming aware of the advantages of fluorescence imaging also translated into wider use across multiple surgical fields.
However, various issues persisted, such as the prohibitive costs of hardware and the requirement for special training, restricting access in some areas.
The industry is expected to maintain its growth trajectory during the upcoming period between 2025 and 2035. North America will continue to lead the way, with a boost from advanced healthcare infrastructure and continuous technological advancements.
The Asia-Pacific region is expected to experience the most rapid growth, fueled by expanded healthcare investments, medical tourism, and an escalating burden of chronic diseases.
Future directions are the creation of new fluorophores for targeted imaging, increasing AI integration to increase diagnostic precision, and broadening applications to other surgical areas.
| Metrics | Values |
|---|---|
| Industry Size (2025E) | USD 758.7 million |
| Industry Value (2035F) | USD 2.225 billion |
| CAGR | 11.9% |
Explore FMI!
Book a free demo
The intraoperative fluorescence imaging industry is on a robust growth path, stimulated by increasing demand for real-time, precision-guided surgery, particularly in oncology and cardiovascular interventions.
Advances such as AI integration and targeted fluorophores are fueling adoption, to the advantage of medtech firms and advanced care providers. Limited equipment affordability and training availability could be roadblocks for smaller hospitals and developing industries.
Invest in AI-Enabled Imaging Solutions
Place emphasis on R&D and collaboration to create AI-enabled fluorescence imaging systems that enhance surgical precision and efficiency, in response to escalating demand for precision medicine.
Grow through Training & Cost Optimization
Realign with industry requirements by offering scalable training and investigating cost-savvy product lines to widen adoption in lower-tier hospitals and developing industries.
Forge Strategic Partnerships and M&A Opportunities
Seek partnerships with surgical device firms and consider acquisitions of specialty imaging startups to drive innovation, expand product lines, and fortify distribution channels around the world.
| Risk | Assessment (Probability - Impact) |
|---|---|
| Regulatory Delays in Approving New Imaging Technologies | Medium - High |
| High Equipment Costs Limiting Adoption in Emerging Industries | High - Medium |
| Shortage of Trained Surgeons and Clinical Staff | Medium - High |
| Priority | Immediate Action |
|---|---|
| Evaluate Emerging Industry Potential | Run feasibility studies on tiered pricing models for cost-sensitive regions. |
| Strengthen Clinical Training Ecosystem | Partner with academic hospitals to launch hands-on surgeon training programs |
| Accelerate Innovation Pipeline | Initiate OEM feedback loop on next-gen AI-integrated imaging system features. |
To remain ahead of the fast-changing intraoperative fluorescence imaging industry, the client needs to shift from incremental innovation to radical, AI-facilitated system development and actively eliminate adoption impediments in unserved industries.
This insight highlights the imperative to redirect the product roadmap to wiser, more accessible imaging products and create a more robust clinical training platform. Strategic capital must be directed toward M&A deals and global distribution partnerships that hasten time-to-industry.
Executives need to see this not only as a growth opportunity, but as a competitive turning point - one in which velocity, integration, and accessibility will shape future leadership in the industry.
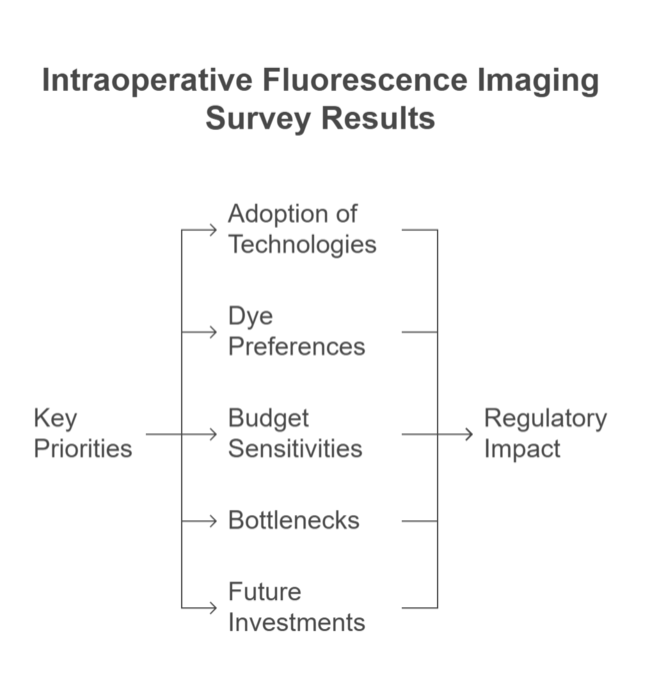
(Surveyed Q4 2024, n=500 stakeholder participants including device manufacturers, surgeons, hospital procurement heads, and regulatory advisors across the USA, Western Europe, Japan, and South Korea)
| Countries | Regulatory Impact and Mandatory Certifications |
|---|---|
| United States | Regulated by the FDA, intraoperative fluorescence imaging systems are typically classified as Class II or III devices. Companies must adhere to stringent Quality System Regulations (QSR) and often require industry approval (PMA) or 510(k) clearance. Clinical data, manufacturing process validation, and labeling compliance are key elements for regulatory approval. Cybersecurity and software integration are becoming increasingly scrutinized. |
| United Kingdom | Post-Brexit, all devices must carry the UKCA (UK Conformity Assessed) mark instead of the CE marking. The MHRA is the regulatory authority responsible for oversight. Manufacturers must undergo conformity assessments, maintain technical documentation, and meet post-industry surveillance requirements. Transitional provisions from CE to UKCA are still in effect for some classes of devices. |
| France | Devices are regulated under the EU Medical Device Regulation (MDR) and require CE marking. The French regulator (ANSM) enforces compliance with clinical evaluation, vigilance, and quality assurance requirements. Manufacturers must follow strict traceability, documentation, and risk management protocols to enter and remain in the French healthcare system. |
| Germany | Germany adheres to the EU MDR framework, and devices must bear CE marking. Regulatory supervision is managed by BfArM. Manufacturers must ensure conformity to safety, performance, and usability standards. German regulators emphasize clinical evidence and post-industry data collection to continuously monitor device safety. |
| Italy | In Italy, devices must comply with EU MDR and be registered with the national health authority. CE marking is required, and Italian-specific device databases must be updated regularly. Documentation of risk-benefit assessments, clinical data, and manufacturer responsibility declarations are mandatory to ensure device traceability and approval. |
| China | The National Medical Products Administration (NMPA) requires both local type testing and administrative approval. Companies must register devices under Chinese classification standards and demonstrate compliance with local technical specifications. A domestic agent is required for foreign manufacturers. Local clinical trials may be required depending on the device class. |
| Japan | Regulated under the PMD Act, devices must be reviewed by the PMDA and receive either approval or certification based on risk class. The regulatory framework mandates safety testing, cybersecurity considerations, and conformity to Japanese Industrial Standards (JIS). Documentation of software integrity and long-term device performance is a key part of the review process. |
| South Korea | Devices are overseen by the MFDS and require Good Manufacturing Practice (GMP) certification. Registration depends on the classification, with higher-risk devices undergoing full technical evaluation. Korea has increased its focus on software safety and clinical outcomes. Manufacturers must submit labeling in Korean and provide local post-industry surveillance support. |
| Australia | The Therapeutic Goods Administration (TGA) mandates that devices be registered in the Australian Register of Therapeutic Goods (ARTG). Manufacturers must demonstrate compliance with Essential Principles, and overseas companies often use EU CE marking or FDA approvals to expedite approval via mutual recognition routes. Post-industry obligations and incident reporting are strictly enforced. |
| New Zealand | Medical devices are regulated by Medsafe under a notification-based system. While not requiring industry approval, all devices must meet safety and performance standards. Manufacturers are encouraged to align with international regulatory frameworks, such as ISO 13485. Post-industry controls, recall procedures, and importer responsibilities are actively monitored. |
| India | Devices are governed by the Medical Device Rules, 2017. Approval is issued by the CDSCO, and registration is mandatory for Class A to D devices. Devices must comply with Indian quality standards and require periodic renewal. Local clinical data may be needed for higher-risk categories. GMP compliance and licensed importing are prerequisites for commercial distribution. |
The USA is expected to be the most profitable industry in the world, backed by sound healthcare infrastructure, high uptake of advanced image modalities, and high clinical research funding. Extensive use of fluorescence-guided surgery (FGS) in oncology and neurological procedures-particularly with indocyanine green (ICG) and 5-ALA-has generated steady demand.
Moreover, device companies in the USA are at the forefront of developing next-generation near-infrared (NIR) systems coupled with robotic platforms, thus driving further innovation. Hospitals are under pressure to enhance surgical accuracy, compelling adoption throughout tertiary care facilities. The FDA's transparent pathways (510(k), PMA) and active digital health guidelines also enable quicker commercialization.
FMI opines that United States Intraoperative Fluorescence Imaging sales are likely to expand at a CAGR of 13.1% during the forecast period between 2025 and 2035.
Committed to the NHS's long-term vision of embracing AI-surgical equipment, the UK industry is recording strong growth in fluorescence imaging solutions. Topnotch university hospitals in Oxford, London, and Manchester are utilizing NIR systems for risky procedures. Post-Brexit regulatory changes under UKCA marking significantly track with MDR, fostering industry continuity in clinical adoption.
There is also added emphasis on decreasing intraoperative complications and hospital stays-aligning with the nation's health efficiency objectives. Investment in digital operating rooms by the private sector is driving adoption at an accelerated rate.
FMI opines that United Kingdom Intraoperative Fluorescence Imaging sales are likely to expand at a CAGR of 13.1% during the forecast period between 2025 and 2035.
France has also become a first adopter of intraoperative imaging devices in cancer surgery, most notably breast cancer and colorectal cancer. State healthcare organizations increasingly support reimbursement for NIR procedures as a stimulus to hospital-level investments.
Public-private collaborations, for example, by the Institut Curie and AP-HP, are piloting AI-fluorescence combined platforms. Very high surgeon acceptance, expanding trial participation, and access to EU R&D monies form the basis for future growth.
FMI opines that France's Intraoperative Fluorescence Imaging sales are likely to expand at a CAGR of 12.5% during the forecast period between 2025 and 2035.
Germany's healthcare infrastructure facilitates the quick deployment of high-precision surgical systems. With several top hospitals incorporating intraoperative NIR imaging into their neurosurgery and hepatobiliary surgery procedures, the industry is growing. German companies are actively working on dual-mode imaging and AI-based systems.
MDR-compliant CE certification and an increasing aging population are other growth drivers. Hospital digitalization grants under "Krankenhauszukunftsgesetz" (KHZG) are also driving improvements in surgical imaging suites.
FMI opines that Germany's Intraoperative Fluorescence Imaging sales are likely to expand at a CAGR of 12.7% during the forecast period between 2025 and 2035.
Italy's uptake is gaining speed through enhanced investment in minimally invasive procedures and cancer treatment centers. Disparities in regional healthcare infrastructure are being tackled by EU recovery funds, which feature digital surgical equipment provisions. Fluorescence imaging is becoming more prevalent in vascular and thyroid operations. Budgetary limitations in the public sector remain a modest obstacle.
FMI opines that Italy's Intraoperative Fluorescence Imaging sales are likely to expand at a CAGR of 12.3% during the forecast period between 2025 and 2035.
South Korea is among the fastest-growing industries in Asia, due to government incentives for medical AI integration and smart hospitals. Hospitals such as Seoul National University Hospital are leading the way in the use of fluorescence in hybrid ORs.
There is an initiative towards local production of ICG and high-end NIR imaging systems, minimizing imports. High digital literacy among clinicians facilitates the rapid adoption of multi-modal and robotic fluorescence platforms.
FMI opines that South Korea's Intraoperative Fluorescence Imaging sales are likely to expand at a CAGR of 13.8% during the forecast period between 2025 and 2035.
Japan is an important industry because of its aging population and culture of precision surgery. The uptake of intraoperative fluorescence is strong in hepatobiliary and lung surgery, with national reimbursement for ICG imaging already established. PMDA approval, though strict, is efficient for established tech.
Japan's research community is actively developing custom imaging agents appropriate for the local population, facilitating uptake.
FMI opines that Japan's Intraoperative Fluorescence Imaging sales are likely to expand at a CAGR of 12.0% during the forecast period between 2025 and 2035.
China is becoming a high-growth industry with increasing surgical volumes and competitive hospital infrastructure growth under the Healthy China 2030 program. Local companies are entering the field of fluorescence imaging, backed by local FDA-equivalent (NMPA) fast-track clearances for AI and imaging-driven innovations. Strong investment in oncology centers is driving demand for NIR fluorescence solutions. Cost-efficient local solutions are expanding access in Tier 2/3 cities.
FMI opines that China's Intraoperative Fluorescence Imaging sales are likely to expand at a CAGR of 12.8% during the forecast period between 2025 and 2035.
Australia and New Zealand are slowly embracing intraoperative fluorescence imaging technologies, with oncology-centric hospitals and research centers leading the way. Reimbursement coverage for fluorescence-guided surgery is still restricted but is likely to increase.
The industry is facilitated by increased visibility into the best practices worldwide and by a drive for robotic surgery adoption, with fluorescence imaging likely to be bundled. Regulation alignment with EU MDR helps facilitate device imports.
FMI opines that Australia & New Zealand Intraoperative Fluorescence Imaging sales are likely to expand at a CAGR of 11.5% during the forecast period between 2025 and 2035.
India's industry is increasing steadily as a result of increased complex cancer surgeries and specialty hospital growth. Adoption is restricted to tier-1 cities as a result of cost sensitivity and the absence of reimbursement channels for fluorescence-guided procedures. Increasing public-private partnerships and the development of domestic device manufacturers are enhancing affordability. Clinical awareness is also on the rise with training programs and medical conferences.
FMI opines that India's Intraoperative Fluorescence Imaging sales are likely to expand at a CAGR of 10.1% during the forecast period between 2025 and 2035.
Between 2025 and 2035, Handheld Fluorescence Imaging Systems will be the most profitable product segment due to their portability, simplicity of intraoperative integration, and growing need for point-of-care surgical visualization.
In contrast to cart-mounted systems, handheld units allow surgeons to reach hard-to-reach anatomical sites and are especially beneficial in minimally invasive and robotically assisted procedures. These systems are less expensive and outpatient-friendly as well, increasing their application in developed and emerging industries alike.
Handheld devices are surgeons' instruments of choice for procedures involving dynamic motion or deeper examination, including sentinel lymph node mapping in skin and breast cancer. As technology miniaturizes further, advances image resolution, and adds wireless data capabilities, adoption is spreading in hospitals and ambulatory surgery centers.
The Handheld Fluorescence Imaging System segment will witness a CAGR of about 13.5% through the forecast period from 2025 to 2035, ahead of the average of the global industry rate of 11.9%.
Between 2025 and 2035, Laser Diodes will be the most profitable light source segment, given their high excitation efficiency, narrow wavelength specificity, and higher signal-to-noise ratio in near-infrared imaging. Laser diodes are specifically best for deep tissue penetration and are hence suitable for high-contrast visualization during intricate surgery procedures.
Surgeons are increasingly opting for systems that incorporate laser diode illumination for increased accuracy in tumor margin identification, vascular mapping, and nerve location.
Moreover, improvements in diode laser miniaturization are facilitating integration within handheld and robotic surgical devices.
As increasing demand for better resolution and real-time feedback in oncology surgery is on the rise, the Laser Diodes segment is expected to register a CAGR of around 12.7% over 2025 to 2035.
Between 2025 and 2035, Cancer Surgery will be the most profitable application segment since the global cancer burden is on the increase and healthcare systems value surgical accuracy to enhance patient outcomes. Fluorescence-guided imaging is essential for tumor margin detection, lymph node mapping, and intraoperative decision-making-core factors in decreasing recurrence and enhancing survival rates.
Growing acceptance of targeted imaging reagents such as 5-ALA and ICG for cancer applications, along with robust clinical evidence demonstrating their effectiveness, is further fueling adoption. The inclusion of imaging technology within robot-assisted oncologic procedures is also fueling fast growth. Growing momentum toward more organ-sparing and minimally invasive forms of cancer surgery will further drive demand for real-time intraoperative visualization.
The Cancer Surgery segment is expected to expand at a CAGR of around 13.2% from 2025 to 2035.
Between 2025 and 2035, Hospitals will continue to be the most profitable end-user segment, mainly because of their advanced surgical infrastructure, presence of multidisciplinary teams, and capability for adopting capital-intensive advanced imaging technologies. Tertiary and quaternary care hospitals are the locations where most complex cancer, cardiovascular, and reconstructive surgeries, making use of intraoperative fluorescence imaging, are carried out.
Also, hospitals are making significant investments in digital ORs and robotic surgical systems, wherein integration of fluorescence is becoming the norm. Government support, reimbursement harmonization, and centralized purchasing are also facilitating adoption in public and private facilities.
The hospital segment is expected to register a growth of around 12.4% CAGR during the forecast period 2025 to 2035.
The industry for intraoperative fluorescence imaging is moderately consolidated, with major players like Stryker Corporation, Olympus Corporation, and Medtronic PLC dominating the industry shares. These players compete based on technological innovation, strategic alliances, and geographic presence. They spend significantly on research and development to launch sophisticated imaging systems that improve surgical accuracy and patient outcomes.
Olympus Corporation in September 2024 introduced the VISERA S, an integrated imaging platform combining high-end diagnostic functions, such as narrow-band imaging (NBI). The system is designed to enhance diagnostic productivity and patient experience in ENT treatment environments.
Also, in January 2024, Karl Storz SE & Co. KG acquired Innersight Labs Ltd., a UK-based firm that deals in AI-driven software for generating 3D models from medical imaging scans. The acquisition is likely to further boost Karl Storz's ability to merge artificial intelligence with surgical imaging technology.
The need for real-time surgical precision and better visualization of tumors, blood vessels, and nerves during surgery is fueling rapid adoption.
Cancer, cardiovascular, and reconstructive surgeries are seeing the highest usage due to enhanced detection and decision-making.
Yes, handheld systems are gaining traction due to their flexibility, cost-efficiency, and suitability for outpatient or minimally invasive procedures.
Advanced light sources, AI-integrated visualization, and imaging agents tailored to specific pathologies are reshaping how surgeries are performed.
Tighter clinical safety standards and faster approvals for imaging agents are accelerating the integration of these systems, especially in oncology-focused health systems.
Cart Based Fluorescence Imaging System, Handheld Fluorescence Imaging Systems, Others
Laser Diodes, Light Emitting Diodes, Filtered Lamp Source
Cancer Surgery, Cardiovascular Surgery, Reconstructive Surgery, Thyroid Surgery, Others
Hospitals, Clinics, Ambulatory Surgical Centers
North America, Latin America, Western Europe, Eastern Europe, East Asia, South Asia & Pacific, Middle East & Africa (MEA)
CGRP Inhibitors Market Trends - Growth, Demand & Forecast 2025 to 2035
Indolent Systemic Mastocytosis treatment Market Insights: Size, Trends & Forecast 2025 to 2035
Lung Cancer PCR Panel Market Trends, Growth, Demand & Forecast 2025 to 2035
Polymyxin Resistance Testing Market Analysis by Product, Testing Methods, End User, and Region - Forecast for 2025 to 2035
Procalcitonin (PCT) Assay Market Analysis by Component, Type, and Region - Forecast for 2025 to 2035
Prostate-Specific Antigen Testing Market Analysis - Size, Share & Forecast 2025 to 2035
Thank you!
You will receive an email from our Business Development Manager. Please be sure to check your SPAM/JUNK folder too.