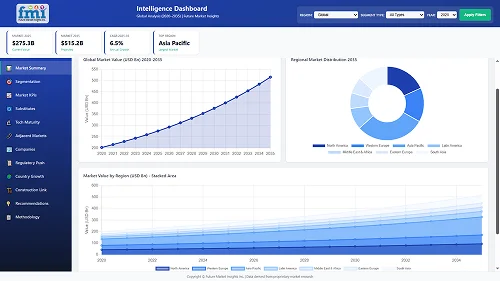
The dyspnea treatment industry will be valued at USD 7.22 billion in 2025. As per FMI's analysis, dyspnea treatment will grow at a CAGR of 6.9% and reach USD 14.06 billion by 2035.
In 2024, the industry grew steadily, driven by innovations in drug delivery technologies and increased demand for respiratory therapy as a result of the growing prevalence of COPD, asthma, and post-COVID lung disorders.
Next-gen inhalers and biologics for severe asthma drove growth. In addition, the wider use of telemedicine enhanced the availability of management, particularly in rural and underserved areas. Moreover, temporary nebulizer shortages arose from supply chain disruptions of nebulizer manufacturing, causing minimal difficulties in some industries.
The worldwide industry for treating this is expected to expand at a consistent 6.9% CAGR to reach USD 7.22 billion in 2025 and grow to USD 14.06 billion in 2035. This growth path will be dominated by four revolutionary trends transforming respiratory therapy. Firstly, the move towards personalized medicine is driving faster uptake of biologics and targeted therapies, especially for resistant patients, which allows for more targeted treatment strategies.
Second, the integration of digital health is transforming patient management with AI-driven remote monitoring devices and smart inhalers that are significantly improving treatment adherence and clinical outcomes.
Third, rising areas in Asia-Pacific and Latin America are reflecting faster growth due to higher investments in healthcare and better access to respiratory therapies. Fourth, the aging of the global population is driving continuous demand as chronic respiratory and cardiovascular diseases are increasing globally.
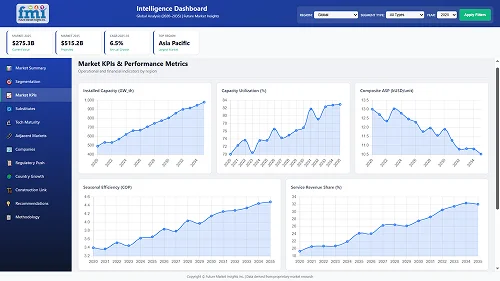
Key Metrics
| Metrics | Values |
|---|---|
| Industry Size (2025E) | USD 7.22 billion |
| Industry Value (2035F) | USD 14.06 billion |
| Value-based CAGR (2025 to 2035) | 6.9% |
(Q4 2024, surveyed n=500 stakeholders: manufacturers, distributors, pulmonologists, and hospital administrators in the USA, Western Europe, Japan, and South Korea)
Regional Difference:
ROI Perceptions:
76% of USA/EU respondents perceived digital adherence tools as "high-return," while 45% in Japan opted for generics at low costs.
Consensus:
70% supported combination inhalers (ICS/LABA) for COPD/asthma on the basis of convenience.
Variance:
Shared Challenges: 91% mentioned drug price pressures (e.g., biologics at USD 20K/year).
Regional Differences:
Manufacturers:
Distributors:
Providers:
Global Alignment: 80% of producers investing in biologics for niche subtypes (e.g., IL-33 inhibitors).
Divergence:
High Consensus:
Demand for cost-effective, evidence-based treatments is global.
Key Variances:
Strategic Insight:
Success depends on regional customization-e.g., digital tools in the USA, biosimilars in Asia, and eco-design in Europe.
| Country/Region | Key Policies & Regulations |
|---|---|
| USA |
|
| European Union |
|
| Japan |
|
| South Korea |
|
| China |
|
| India |
|
The global industry is expected to grow steadily (6.9% CAGR) due to increasing COPD/asthma prevalence, aging, and digital health adoption. Biologic developers, intelligent inhaler producers, and telemedicine vendors will gain the most, while generic producers and struggling incumbents are subjected to margin squeezes due to pricing reforms and sustainability requirements. Winners will be region-based on regulatory adaptability (e.g., USA/EU biologics, Asia cost-effective generics).
Prioritize precision Medicine & Biologics
Invest in high-value targeted treatments (e.g., IL-5/IL-33 inhibitors) for more severe asthma/COPD subtypes, supported by companion diagnostic tests to validate cost-effectiveness to payers. Invest R&D in biosimilars in price-conscious areas (e.g., Asia) and gene therapies for specialty indications (e.g., alpha-1 antitrypsin deficiency).
Lead the Digital Health Integration Wave
Create AI-based solutions (e.g., smart inhalers with adherence monitoring and exacerbation prediction algorithms) and collaborate with telehealth platforms to monetize value in remote monitoring. Emphasize FDA/EU-compliant data privacy and reimbursement strategy (e.g., CPT codes for digital therapeutics).
Maximize Regional Commercialization Models
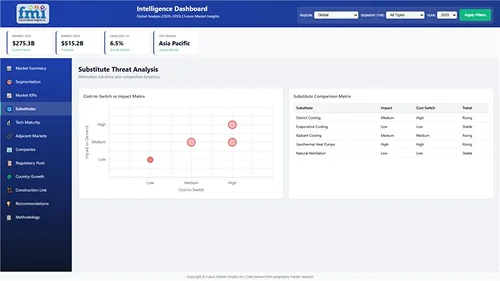
| Risk | Probability |
|---|---|
| Drug Pricing Reforms (e.g., USA IRA negotiations, EU cost-effectiveness mandates) | High |
| Propellant Phase-Outs (EPA/EU bans on HFA inhalers by 2025 to 2035) | Medium |
| Digital Health Adoption Lag (Slow clinician uptake and reimbursement hurdles for AI tools) | Medium |
| Priority | Immediate Action |
|---|---|
| Accelerate Biologic Subtype Expansion | Launch feasibility studies for IL-33/TSLP inhibitors in severe COPD (target 2-3 pipeline candidates by Q4). |
| Navigate Inhaler Propellant Transition | Secure supply contracts for next-gen HFO propellants; initiate FDA/EMA pre-submission meetings for reformulations. |
| Scale Digital Therapeutics Adoption | Partner with 3-5 telehealth platforms (e.g., Teladoc, Amwell) to bundle smart inhalers with remote monitoring services. |
| Optimize Emerging Pricing | Pilot tiered pricing models in India/Southeast Asia (e.g., USD 10-50/month generics) via local manufacturing JVs. |
| Mitigate IRA-Driven Margin Risks | Diversify into non-reimbursed digital health (e.g., direct-to-consumer asthma coaching subscriptions). |
To stay ahead, companies in the industry are poised to hit USD 14 billion by 2035, fueled by an aging population, increasing COPD/asthma incidence, and digital health technology.
To gain a leadership position, we suggest an urgent strategic redirection of 20% of R&D investment into precision biologics for refractory subtypes, specifically, IL-33 and TSLP inhibitors for eosinophil-negative patients, a high-value niche presently under-treated by generic LABA/ICS therapies.
At the same time, we suggest acquiring or forming a partnership with a smart inhaler analytics startup (e.g., Propeller Health competitors) to add AI-powered adherence monitoring to our portfolio, building a closed-loop respiratory care system.
Supplemental oxygen therapy is the most common therapy for dyspnea worldwide, especially for chronic respiratory diseases such as COPD, pulmonary fibrosis, and end-stage heart failure. It has become so prominent in practice due to its power to instantaneously alleviate breathlessness by immediately addressing hypoxemia (hypoxygenation) directly, which is frequently the pathophysiological basis for breathlessness in such patients.
As compared to drugs, whose action takes days to manifest and whose response may be unpredictable, oxygen therapy ensures quick and quantifiable improvement in oxygenation status and symptom abatement.
Strict clinical guidelines across hospitals, home care, and palliative settings are supported by the universal availability of the therapy, including, for example, the GOLD guidelines for COPD, which provide a mandate to use it as soon as certain blood oxygen level thresholds are dropped.
This renders oxygen therapy an absolute intervention in the case of severe instances. At the same time, other medications such as anticholinergics or corticosteroids are condition-based and have risks of side effects with prolonged administration.
Inhaled treatments are much more prevalent than oral drugs in the treatment of dyspnea, especially in chronic respiratory disorders such as asthma and COPD, because of a number of important benefits. The most significant advantage of inhalation therapy is its direct deposition of medication within the lungs, which enables quick onset of action and increased local drug concentration with much reduced systemic side effects compared to oral delivery.
For corticosteroids and bronchodilators - the cornerstone therapies for obstructive lung conditions - inhalation offers instant relief by acting on the airways exactly where they are needed. At the same time, oral forms of these medications would have to be taken in much larger amounts in order to have equivalent lung action, inviting danger such as oral thrush, hoarseness, or systemic side effects like osteoporosis with steroids.
Hospitals are still the most common environment for dyspnea treatment across the world, acting as the first line of care for acute and severe respiratory conditions. This is due to their extensive facilities in handling critical dyspnea attacks through emergency rooms, ICUs, and specialized pulmonary units with advanced diagnostics, oxygen therapy equipment, and ventilator support.
Though home care has expanded dramatically for chronic diseases such as COPD - driven by portable oxygen concentrators and telehealth monitoring - hospitals retain irreplaceable strengths: 24/7 access to pulmonologists, capacity to manage life-threatening exacerbations, and facilities for complicated testing (CT scans, bronchoscopies).
| Countries | CAGR |
|---|---|
| USA | 6.5% |
| UK | 5.8% |
| France | 5.6% |
| Germany | 6.0% |
| Italy | 5.4% |
| South Korea | 6.2% |
| Japan | 5.5% |
| China | 7.0% |
The USA is expected to observe a CAGR of around 6.5% for the treatment of dyspnea between the years 2025 and 2035. This is driven by a widespread prevalence of respiratory disorders like chronic obstructive pulmonary disease (COPD) and asthma.
More than 25 million people in the USA suffer from asthma, and nearly 14.8 million adults have been diagnosed with COPD, as stated by the Office of Disease Prevention and Health Promotion. Advanced healthcare infrastructure, high healthcare spending, and continued research and development activities further boost the size. In addition, the rise in the adoption of new therapies and government support toward enhancing respiratory wellness is anticipated to drive growth.
The UK’s industry is estimated to expand at a CAGR of approximately 5.8% from 2025 to 2035. The growth in the prevalence of respiratory disorders, combined with population aging, highlights the need for successful treatments.
The National Health Service (NHS) offers a strong infrastructure for the uptake of innovative therapies, and repeated public health campaigns emphasize early diagnosis and treatment of respiratory diseases. Academic institution-pharmaceutical company collaborations are encouraging treatment innovation and driving further expansion.
France's industry is likely to witness a CAGR of around 5.6% during the forecast period. The nation's well-developed healthcare infrastructure and focus on preventive care help in the early diagnosis and treatment of respiratory diseases.
Government programs aimed at lowering the number of smokers and enhancing air quality are favorably affecting the incidence of respiratory diseases. Furthermore, France's robust pharma industry is actively involved in the creation of new therapies for dyspnea, boosting the treatment paradigm.
Germany is also expected to grow at a CAGR of around 6.0% during the industry period of 2025 to 2035. The advanced healthcare infrastructure and high healthcare spending in the country enable access to innovative treatments.
Germany's emphasis on research and development, especially in respiratory care, has resulted in the launch of new therapies. The rising incidence of respiratory diseases, partially caused by environmental conditions, also contributes to the growth in demand for effective treatments.
Italy's industry is expected to register a CAGR of around 5.4% over the forecast period. The elderly population in Italy is one of the key drivers of the increasing prevalence of respiratory diseases. The Italian healthcare system's focus on offering comprehensive care means that patients receive the treatments they need.
Public health programs that help promote respiratory well-being and decrease pollution levels are also expected to have a positive impact on market growth.
The South Korean industry is anticipated to exhibit a CAGR of approximately 6.2% during the forecast period from 2025 to 2035. Increased air pollution due to fast urbanization and industrialization has fueled the incidence of respiratory diseases.
The healthcare infrastructure investments made by the government of South Korea and the focus on the implementation of advanced medical technology are supporting more effective diagnosis and treatment of dyspnea. In addition, the nation's expanding pharma industry is aggressively engaged in bringing novel treatments to the market and developing them.
Japan is expected to witness a CAGR of around 5.5% in the industry over the forecast period. Japan's super-aged society has a high prevalence of chronic diseases, such as respiratory diseases.
Japan's healthcare system is universal in coverage and has a strong preventive care focus, allowing for early intervention for dyspnea. Advances in technology and personalized medicine are also improving treatment outcomes for respiratory patients.
The industry in China is expected to expand with a strong CAGR of approximately 7.0% between 2025 and 2035. The huge population and rising incidence of respiratory conditions, fueled by environmental pollution and smoking, are key drivers for the market growth in China.
The initiatives of the Chinese government towards healthcare reform, insurance expansion, and investment in the medical infrastructure are enhancing the availability of treatments. In addition, China's rising pharmaceutical sector is also playing a significant part in the creation and dissemination of respiratory therapies.
GSK (25% share):
Leads with Trelegy Ellipta (asthma/COPD) and Advair, riding on its respiratory franchise.
AstraZeneca (20%):
Leader in biologics (Fasenra for eosinophilic asthma) and Symbicort (ICS/LABA).
Boehringer Ingelheim (15%):
Major player with Spiriva (tiotropium) and Ofev (IPF).
Novartis (10%):
Concentrated on Xolair (allergic asthma) and Enerzair (smart inhaler combination).
Philips Respironics (30%):
Hospital nebulizer (e.g., Innospire) and portable oxygen concentrator leader.
Vectura Group (20%):
Dry powder inhalers (collaborating with GSK, Novartis).
Omron Healthcare (15%):
Home nebulizers (Japan/Asia focus).
PARI Pharma (10%):
Specialty leader in eFlow digital nebulizers.
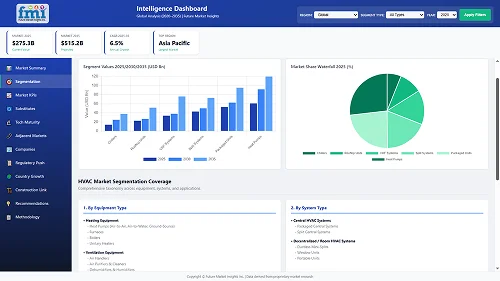
With respect to the treatment, it is classified into therapy, supplemental oxygen therapy, relaxation therapy, drugs, antianxiety drugs, antibiotics, anticholinergic agents, corticosteroids, and others.
In terms of route of administration, it is divided into oral, inhalation, and others.
In terms of end-users, it is divided into hospitals, home care, and speciality centres.
In terms of region, it is segmented into North America, Latin America, Europe, East Asia, South Asia, Oceania, and MEA.
The most frequently prescribed are inhaled bronchodilators, corticosteroids, and supplemental oxygen therapy.
They monitor medication use and notify physicians about deteriorating symptoms through a Bluetooth connection.
They treat precise inflammation pathways in severe asthma/COPD with fewer side effects than steroids.
The USA, EU countries, and China because of lung diseases associated with aging and pollution.
Gene therapies for uncommon lung disorders and AI-driven symptom forecasters hold the greatest promise.
Table 1: Global Market Value (US$ Million) Forecast by Region, 2018 to 2033
Table 2: Global Market Value (US$ Million) Forecast by Treatment, 2018 to 2033
Table 3: Global Market Value (US$ Million) Forecast by Route of Administration, 2018 to 2033
Table 4: Global Market Value (US$ Million) Forecast by End-user, 2018 to 2033
Table 5: North America Market Value (US$ Million) Forecast by Country, 2018 to 2033
Table 6: North America Market Value (US$ Million) Forecast by Treatment, 2018 to 2033
Table 7: North America Market Value (US$ Million) Forecast by Route of Administration, 2018 to 2033
Table 8: North America Market Value (US$ Million) Forecast by End-user, 2018 to 2033
Table 9: Latin America Market Value (US$ Million) Forecast by Country, 2018 to 2033
Table 10: Latin America Market Value (US$ Million) Forecast by Treatment, 2018 to 2033
Table 11: Latin America Market Value (US$ Million) Forecast by Route of Administration, 2018 to 2033
Table 12: Latin America Market Value (US$ Million) Forecast by End-user, 2018 to 2033
Table 13: Europe Market Value (US$ Million) Forecast by Country, 2018 to 2033
Table 14: Europe Market Value (US$ Million) Forecast by Treatment, 2018 to 2033
Table 15: Europe Market Value (US$ Million) Forecast by Route of Administration, 2018 to 2033
Table 16: Europe Market Value (US$ Million) Forecast by End-user, 2018 to 2033
Table 17: South Asia Market Value (US$ Million) Forecast by Country, 2018 to 2033
Table 18: South Asia Market Value (US$ Million) Forecast by Treatment, 2018 to 2033
Table 19: South Asia Market Value (US$ Million) Forecast by Route of Administration, 2018 to 2033
Table 20: South Asia Market Value (US$ Million) Forecast by End-user, 2018 to 2033
Table 21: East Asia Market Value (US$ Million) Forecast by Country, 2018 to 2033
Table 22: East Asia Market Value (US$ Million) Forecast by Treatment, 2018 to 2033
Table 23: East Asia Market Value (US$ Million) Forecast by Route of Administration, 2018 to 2033
Table 24: East Asia Market Value (US$ Million) Forecast by End-user, 2018 to 2033
Table 25: Oceania Market Value (US$ Million) Forecast by Country, 2018 to 2033
Table 26: Oceania Market Value (US$ Million) Forecast by Treatment, 2018 to 2033
Table 27: Oceania Market Value (US$ Million) Forecast by Route of Administration, 2018 to 2033
Table 28: Oceania Market Value (US$ Million) Forecast by End-user, 2018 to 2033
Table 29: MEA Market Value (US$ Million) Forecast by Country, 2018 to 2033
Table 30: MEA Market Value (US$ Million) Forecast by Treatment, 2018 to 2033
Table 31: MEA Market Value (US$ Million) Forecast by Route of Administration, 2018 to 2033
Table 32: MEA Market Value (US$ Million) Forecast by End-user, 2018 to 2033
Figure 1: Global Market Value (US$ Million) by Treatment, 2023 to 2033
Figure 2: Global Market Value (US$ Million) by Route of Administration, 2023 to 2033
Figure 3: Global Market Value (US$ Million) by End-user, 2023 to 2033
Figure 4: Global Market Value (US$ Million) by Region, 2023 to 2033
Figure 5: Global Market Value (US$ Million) Analysis by Region, 2018 to 2033
Figure 6: Global Market Value Share (%) and BPS Analysis by Region, 2023 to 2033
Figure 7: Global Market Y-o-Y Growth (%) Projections by Region, 2023 to 2033
Figure 8: Global Market Value (US$ Million) Analysis by Treatment, 2018 to 2033
Figure 9: Global Market Value Share (%) and BPS Analysis by Treatment, 2023 to 2033
Figure 10: Global Market Y-o-Y Growth (%) Projections by Treatment, 2023 to 2033
Figure 11: Global Market Value (US$ Million) Analysis by Route of Administration, 2018 to 2033
Figure 12: Global Market Value Share (%) and BPS Analysis by Route of Administration, 2023 to 2033
Figure 13: Global Market Y-o-Y Growth (%) Projections by Route of Administration, 2023 to 2033
Figure 14: Global Market Value (US$ Million) Analysis by End-user, 2018 to 2033
Figure 15: Global Market Value Share (%) and BPS Analysis by End-user, 2023 to 2033
Figure 16: Global Market Y-o-Y Growth (%) Projections by End-user, 2023 to 2033
Figure 17: Global Market Attractiveness by Treatment, 2023 to 2033
Figure 18: Global Market Attractiveness by Route of Administration, 2023 to 2033
Figure 19: Global Market Attractiveness by End-user, 2023 to 2033
Figure 20: Global Market Attractiveness by Region, 2023 to 2033
Figure 21: North America Market Value (US$ Million) by Treatment, 2023 to 2033
Figure 22: North America Market Value (US$ Million) by Route of Administration, 2023 to 2033
Figure 23: North America Market Value (US$ Million) by End-user, 2023 to 2033
Figure 24: North America Market Value (US$ Million) by Country, 2023 to 2033
Figure 25: North America Market Value (US$ Million) Analysis by Country, 2018 to 2033
Figure 26: North America Market Value Share (%) and BPS Analysis by Country, 2023 to 2033
Figure 27: North America Market Y-o-Y Growth (%) Projections by Country, 2023 to 2033
Figure 28: North America Market Value (US$ Million) Analysis by Treatment, 2018 to 2033
Figure 29: North America Market Value Share (%) and BPS Analysis by Treatment, 2023 to 2033
Figure 30: North America Market Y-o-Y Growth (%) Projections by Treatment, 2023 to 2033
Figure 31: North America Market Value (US$ Million) Analysis by Route of Administration, 2018 to 2033
Figure 32: North America Market Value Share (%) and BPS Analysis by Route of Administration, 2023 to 2033
Figure 33: North America Market Y-o-Y Growth (%) Projections by Route of Administration, 2023 to 2033
Figure 34: North America Market Value (US$ Million) Analysis by End-user, 2018 to 2033
Figure 35: North America Market Value Share (%) and BPS Analysis by End-user, 2023 to 2033
Figure 36: North America Market Y-o-Y Growth (%) Projections by End-user, 2023 to 2033
Figure 37: North America Market Attractiveness by Treatment, 2023 to 2033
Figure 38: North America Market Attractiveness by Route of Administration, 2023 to 2033
Figure 39: North America Market Attractiveness by End-user, 2023 to 2033
Figure 40: North America Market Attractiveness by Country, 2023 to 2033
Figure 41: Latin America Market Value (US$ Million) by Treatment, 2023 to 2033
Figure 42: Latin America Market Value (US$ Million) by Route of Administration, 2023 to 2033
Figure 43: Latin America Market Value (US$ Million) by End-user, 2023 to 2033
Figure 44: Latin America Market Value (US$ Million) by Country, 2023 to 2033
Figure 45: Latin America Market Value (US$ Million) Analysis by Country, 2018 to 2033
Figure 46: Latin America Market Value Share (%) and BPS Analysis by Country, 2023 to 2033
Figure 47: Latin America Market Y-o-Y Growth (%) Projections by Country, 2023 to 2033
Figure 48: Latin America Market Value (US$ Million) Analysis by Treatment, 2018 to 2033
Figure 49: Latin America Market Value Share (%) and BPS Analysis by Treatment, 2023 to 2033
Figure 50: Latin America Market Y-o-Y Growth (%) Projections by Treatment, 2023 to 2033
Figure 51: Latin America Market Value (US$ Million) Analysis by Route of Administration, 2018 to 2033
Figure 52: Latin America Market Value Share (%) and BPS Analysis by Route of Administration, 2023 to 2033
Figure 53: Latin America Market Y-o-Y Growth (%) Projections by Route of Administration, 2023 to 2033
Figure 54: Latin America Market Value (US$ Million) Analysis by End-user, 2018 to 2033
Figure 55: Latin America Market Value Share (%) and BPS Analysis by End-user, 2023 to 2033
Figure 56: Latin America Market Y-o-Y Growth (%) Projections by End-user, 2023 to 2033
Figure 57: Latin America Market Attractiveness by Treatment, 2023 to 2033
Figure 58: Latin America Market Attractiveness by Route of Administration, 2023 to 2033
Figure 59: Latin America Market Attractiveness by End-user, 2023 to 2033
Figure 60: Latin America Market Attractiveness by Country, 2023 to 2033
Figure 61: Europe Market Value (US$ Million) by Treatment, 2023 to 2033
Figure 62: Europe Market Value (US$ Million) by Route of Administration, 2023 to 2033
Figure 63: Europe Market Value (US$ Million) by End-user, 2023 to 2033
Figure 64: Europe Market Value (US$ Million) by Country, 2023 to 2033
Figure 65: Europe Market Value (US$ Million) Analysis by Country, 2018 to 2033
Figure 66: Europe Market Value Share (%) and BPS Analysis by Country, 2023 to 2033
Figure 67: Europe Market Y-o-Y Growth (%) Projections by Country, 2023 to 2033
Figure 68: Europe Market Value (US$ Million) Analysis by Treatment, 2018 to 2033
Figure 69: Europe Market Value Share (%) and BPS Analysis by Treatment, 2023 to 2033
Figure 70: Europe Market Y-o-Y Growth (%) Projections by Treatment, 2023 to 2033
Figure 71: Europe Market Value (US$ Million) Analysis by Route of Administration, 2018 to 2033
Figure 72: Europe Market Value Share (%) and BPS Analysis by Route of Administration, 2023 to 2033
Figure 73: Europe Market Y-o-Y Growth (%) Projections by Route of Administration, 2023 to 2033
Figure 74: Europe Market Value (US$ Million) Analysis by End-user, 2018 to 2033
Figure 75: Europe Market Value Share (%) and BPS Analysis by End-user, 2023 to 2033
Figure 76: Europe Market Y-o-Y Growth (%) Projections by End-user, 2023 to 2033
Figure 77: Europe Market Attractiveness by Treatment, 2023 to 2033
Figure 78: Europe Market Attractiveness by Route of Administration, 2023 to 2033
Figure 79: Europe Market Attractiveness by End-user, 2023 to 2033
Figure 80: Europe Market Attractiveness by Country, 2023 to 2033
Figure 81: South Asia Market Value (US$ Million) by Treatment, 2023 to 2033
Figure 82: South Asia Market Value (US$ Million) by Route of Administration, 2023 to 2033
Figure 83: South Asia Market Value (US$ Million) by End-user, 2023 to 2033
Figure 84: South Asia Market Value (US$ Million) by Country, 2023 to 2033
Figure 85: South Asia Market Value (US$ Million) Analysis by Country, 2018 to 2033
Figure 86: South Asia Market Value Share (%) and BPS Analysis by Country, 2023 to 2033
Figure 87: South Asia Market Y-o-Y Growth (%) Projections by Country, 2023 to 2033
Figure 88: South Asia Market Value (US$ Million) Analysis by Treatment, 2018 to 2033
Figure 89: South Asia Market Value Share (%) and BPS Analysis by Treatment, 2023 to 2033
Figure 90: South Asia Market Y-o-Y Growth (%) Projections by Treatment, 2023 to 2033
Figure 91: South Asia Market Value (US$ Million) Analysis by Route of Administration, 2018 to 2033
Figure 92: South Asia Market Value Share (%) and BPS Analysis by Route of Administration, 2023 to 2033
Figure 93: South Asia Market Y-o-Y Growth (%) Projections by Route of Administration, 2023 to 2033
Figure 94: South Asia Market Value (US$ Million) Analysis by End-user, 2018 to 2033
Figure 95: South Asia Market Value Share (%) and BPS Analysis by End-user, 2023 to 2033
Figure 96: South Asia Market Y-o-Y Growth (%) Projections by End-user, 2023 to 2033
Figure 97: South Asia Market Attractiveness by Treatment, 2023 to 2033
Figure 98: South Asia Market Attractiveness by Route of Administration, 2023 to 2033
Figure 99: South Asia Market Attractiveness by End-user, 2023 to 2033
Figure 100: South Asia Market Attractiveness by Country, 2023 to 2033
Figure 101: East Asia Market Value (US$ Million) by Treatment, 2023 to 2033
Figure 102: East Asia Market Value (US$ Million) by Route of Administration, 2023 to 2033
Figure 103: East Asia Market Value (US$ Million) by End-user, 2023 to 2033
Figure 104: East Asia Market Value (US$ Million) by Country, 2023 to 2033
Figure 105: East Asia Market Value (US$ Million) Analysis by Country, 2018 to 2033
Figure 106: East Asia Market Value Share (%) and BPS Analysis by Country, 2023 to 2033
Figure 107: East Asia Market Y-o-Y Growth (%) Projections by Country, 2023 to 2033
Figure 108: East Asia Market Value (US$ Million) Analysis by Treatment, 2018 to 2033
Figure 109: East Asia Market Value Share (%) and BPS Analysis by Treatment, 2023 to 2033
Figure 110: East Asia Market Y-o-Y Growth (%) Projections by Treatment, 2023 to 2033
Figure 111: East Asia Market Value (US$ Million) Analysis by Route of Administration, 2018 to 2033
Figure 112: East Asia Market Value Share (%) and BPS Analysis by Route of Administration, 2023 to 2033
Figure 113: East Asia Market Y-o-Y Growth (%) Projections by Route of Administration, 2023 to 2033
Figure 114: East Asia Market Value (US$ Million) Analysis by End-user, 2018 to 2033
Figure 115: East Asia Market Value Share (%) and BPS Analysis by End-user, 2023 to 2033
Figure 116: East Asia Market Y-o-Y Growth (%) Projections by End-user, 2023 to 2033
Figure 117: East Asia Market Attractiveness by Treatment, 2023 to 2033
Figure 118: East Asia Market Attractiveness by Route of Administration, 2023 to 2033
Figure 119: East Asia Market Attractiveness by End-user, 2023 to 2033
Figure 120: East Asia Market Attractiveness by Country, 2023 to 2033
Figure 121: Oceania Market Value (US$ Million) by Treatment, 2023 to 2033
Figure 122: Oceania Market Value (US$ Million) by Route of Administration, 2023 to 2033
Figure 123: Oceania Market Value (US$ Million) by End-user, 2023 to 2033
Figure 124: Oceania Market Value (US$ Million) by Country, 2023 to 2033
Figure 125: Oceania Market Value (US$ Million) Analysis by Country, 2018 to 2033
Figure 126: Oceania Market Value Share (%) and BPS Analysis by Country, 2023 to 2033
Figure 127: Oceania Market Y-o-Y Growth (%) Projections by Country, 2023 to 2033
Figure 128: Oceania Market Value (US$ Million) Analysis by Treatment, 2018 to 2033
Figure 129: Oceania Market Value Share (%) and BPS Analysis by Treatment, 2023 to 2033
Figure 130: Oceania Market Y-o-Y Growth (%) Projections by Treatment, 2023 to 2033
Figure 131: Oceania Market Value (US$ Million) Analysis by Route of Administration, 2018 to 2033
Figure 132: Oceania Market Value Share (%) and BPS Analysis by Route of Administration, 2023 to 2033
Figure 133: Oceania Market Y-o-Y Growth (%) Projections by Route of Administration, 2023 to 2033
Figure 134: Oceania Market Value (US$ Million) Analysis by End-user, 2018 to 2033
Figure 135: Oceania Market Value Share (%) and BPS Analysis by End-user, 2023 to 2033
Figure 136: Oceania Market Y-o-Y Growth (%) Projections by End-user, 2023 to 2033
Figure 137: Oceania Market Attractiveness by Treatment, 2023 to 2033
Figure 138: Oceania Market Attractiveness by Route of Administration, 2023 to 2033
Figure 139: Oceania Market Attractiveness by End-user, 2023 to 2033
Figure 140: Oceania Market Attractiveness by Country, 2023 to 2033
Figure 141: MEA Market Value (US$ Million) by Treatment, 2023 to 2033
Figure 142: MEA Market Value (US$ Million) by Route of Administration, 2023 to 2033
Figure 143: MEA Market Value (US$ Million) by End-user, 2023 to 2033
Figure 144: MEA Market Value (US$ Million) by Country, 2023 to 2033
Figure 145: MEA Market Value (US$ Million) Analysis by Country, 2018 to 2033
Figure 146: MEA Market Value Share (%) and BPS Analysis by Country, 2023 to 2033
Figure 147: MEA Market Y-o-Y Growth (%) Projections by Country, 2023 to 2033
Figure 148: MEA Market Value (US$ Million) Analysis by Treatment, 2018 to 2033
Figure 149: MEA Market Value Share (%) and BPS Analysis by Treatment, 2023 to 2033
Figure 150: MEA Market Y-o-Y Growth (%) Projections by Treatment, 2023 to 2033
Figure 151: MEA Market Value (US$ Million) Analysis by Route of Administration, 2018 to 2033
Figure 152: MEA Market Value Share (%) and BPS Analysis by Route of Administration, 2023 to 2033
Figure 153: MEA Market Y-o-Y Growth (%) Projections by Route of Administration, 2023 to 2033
Figure 154: MEA Market Value (US$ Million) Analysis by End-user, 2018 to 2033
Figure 155: MEA Market Value Share (%) and BPS Analysis by End-user, 2023 to 2033
Figure 156: MEA Market Y-o-Y Growth (%) Projections by End-user, 2023 to 2033
Figure 157: MEA Market Attractiveness by Treatment, 2023 to 2033
Figure 158: MEA Market Attractiveness by Route of Administration, 2023 to 2033
Figure 159: MEA Market Attractiveness by End-user, 2023 to 2033
Figure 160: MEA Market Attractiveness by Country, 2023 to 2033
Full Research Suite comprises of:
Market outlook & trends analysis
Interviews & case studies
Strategic recommendations
Vendor profiles & capabilities analysis
5-year forecasts
8 regions and 60+ country-level data splits
Market segment data splits
12 months of continuous data updates
DELIVERED AS:
PDF EXCEL ONLINE
Treatment-Resistant Hypertension Management Market Size and Share Forecast Outlook 2025 to 2035
Treatment-Resistant Depression Treatment Market Size and Share Forecast Outlook 2025 to 2035
Treatment Pumps Market Insights Growth & Demand Forecast 2025 to 2035
Pretreatment Coatings Market Size and Share Forecast Outlook 2025 to 2035
Air Treatment Ozone Generator Market Size and Share Forecast Outlook 2025 to 2035
CNS Treatment and Therapy Market Insights - Trends & Growth Forecast 2025 to 2035
Seed Treatment Materials Market Size and Share Forecast Outlook 2025 to 2035
Acne Treatment Solutions Market Size and Share Forecast Outlook 2025 to 2035
Scar Treatment Market Overview - Growth & Demand Forecast 2025 to 2035
Soil Treatment Chemicals Market
Water Treatment System Market Size and Share Forecast Outlook 2025 to 2035
Water Treatment Chemical Market Size and Share Forecast Outlook 2025 to 2035
Algae Treatment Chemical Market Forecast and Outlook 2025 to 2035
Water Treatment Market Size and Share Forecast Outlook 2025 to 2035
Water Treatment Ozone Generator Market Size and Share Forecast Outlook 2025 to 2035
Water Treatment Equipment Market Size and Share Forecast Outlook 2025 to 2035
Burns Treatment Market Overview – Growth, Demand & Forecast 2025 to 2035
CRBSI Treatment Market Insights - Growth, Trends & Forecast 2025 to 2035
Water Treatment Polymers Market Growth & Demand 2025 to 2035
Asthma Treatment Market Forecast and Outlook 2025 to 2035
Thank you!
You will receive an email from our Business Development Manager. Please be sure to check your SPAM/JUNK folder too.
Chat With
MaRIA