The sales of Computer Assisted Coding Software are estimated to be worth USD 6.5 billion in 2025 and are anticipated to reach a value of USD 15.8 billion by 2035. Sales are projected to rise at a CAGR of 10.3% over the forecast period between 2025 and 2035. The revenue generated by Computer Assisted Coding Software in 2024 was USD 5.4 billion. The market is anticipated to exhibit a Y-o-Y growth of 10.3% in 2025.
The adoption of digital healthcare causes the global computer-assisted coding (CAC) software market to accelerate toward becoming a more mature marketplace. CAC software applies AI and natural language processing (NLP) to robotize code allocation processes, thereby significantly enhancing medical coding accuracy and efficiency. With this, accelerating healthcare costs, as well as the need to comply with regulation, are spurring the marketplace forward.
The increasing demand for precise medical records, documentation, and billing is a chief driver. Medical professionals are confronted with the sheer volume of patient data they must process while also maintaining compliance with evolving coding practices like ICD-10 and CPT. CAC software streamlines coding activities, reducing errors and enhancing reimbursement precision.
The marriage of machine learning and artificial intelligence AI is offering significant opportunities. The charting of AI-driven analytics enhances coding accuracy and speed, diminishing human interventions. In contrast, the wider adoption of Cloud-powered CAC software also translates to more affordable choices for healthcare providers, particularly if they expand into new regions.
North America gains the largest share with the help of stringent healthcare regulations, electronic health records already widely in use(EHR), and technology ahead of the rest of the world by a mile. Europe is second, with new digital health infrastructure coming online every day. The Asia-Pacific region, while lagging now, appears poised soon to catch up as national governments within this third-world age focus more and more on health.
Key leaders are investing in AI-based coding tools and strategic alliances to enhance their software strength even more. At the same time, the competitive environment is defined by mergers and acquisitions firms that seek to complete voids in their IT systems offerings and make them more compatible with each other as well.
The leading players include Anderson World Software, EPSi, HALYARD, Inc., and 3M. Anderson's is a full-service company that provides a full range of products, including software solutions for the entire programming process. Gallup will survey the world's most successful IT system this year and will contrast those results strongly with the polls in almost every nation as our database grows.
With healthcare systems across the globe turning to automation and precision-based documentation, the industry is anticipated to boom. AI advancements, regulatory requirements, and the expanding need for data-driven decision-making in medical coding and billing practices will influence future growth.
Computer Assisted Coding Software Market Assessment
| Attributes | Key Insights |
|---|---|
| Industry Size,2025 | USD 6.5 billion |
| Industry Size,2035 | USD 15.8 billion |
| CAGR (2025 to 2035) | 10.3% |
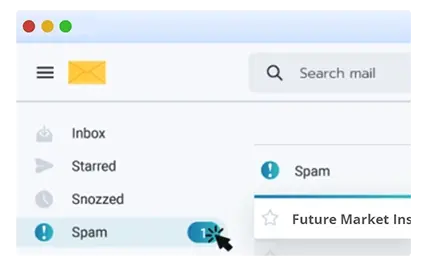
Explore FMI!
Book a free demo
The industry is growing at a rapid rate because of key drivers like increasing regulatory requirements, the complexity of medical coding, and healthcare digitization. The demand for automation in medical coding is particularly high in hospitals and medical billing companies where accuracy and adherence to ICD-10 and CPT coding guidelines are crucial
Artificial Intelligence (AI)-based CAC solutions are becoming increasingly popular, improving coding productivity, accuracy, and revenue cycle management. Integration with Electronic Health Records (EHRs) is an important buying criterion, as seamless interoperability eliminates manual work and enhances coding productivity.
Ambulatory surgical centers and specialty clinics are implementing budget-friendly CAC solutions that provide tailored coding support for outpatient care. Research centers utilize CAC tools mainly to analyze clinical data and conduct population health studies. With automation being a major focus for healthcare organizations, vendors are emphasizing AI-driven coding solutions to minimize claim denials, provide regulatory compliance, and maximize the reimbursement process.
From 2020 to 2024, the sales of CAC software grew rapidly due to the increasing complexity of medical coding, regulatory compliance requirements, and the shift toward value-based healthcare. The growth of electronic health records (EHR) adoption and the necessity of correct medical billing created a demand for artificial intelligence-based coding solutions, minimizing human error and maximizing coding productivity.
Healthcare industry majors like 3M, Optum, and Nuance (Microsoft) brought in natural language processing (NLP) computer-assisted coding (CAC) solutions that allowed hospitals and clinics to automate the coding of ICD-10, CPT, and HCPCS.
Telehealth treatment during the pandemic generated additional burdens on cloud-based computer-assisted coding (CAC) software to support remote medical documentation. Deployment was also hampered by challenges such as integration challenges with existing environments, implementation costs, and resistance from medical personnel in smaller medical facilities.
From 2025 to 2035, the industry will be dominated by AI-powered automation, blockchain-secured security, and real-time predictive analytics. Deep learning algorithms with advanced complexities will make CAC systems context-sensitive, help them identify fraud, and correct errors automatically during medical recordation, reducing denials.
Blockchain will guarantee improved data security and compliance monitoring, discouraging the unauthorized alteration of patient records.Integration of speech recognition with AI will make coding on the fly as physicians communicate, cutting administrative burdens.
Epic Systems and Cernerwill design completely interoperable CAC systems that seamlessly communicate with hospital information systems (HIS) and insurance databases. Predictive analytics will make it possible to proactively manage revenue cycles to identify potential billing irregularities before claims submission.
The beginning of autonomous coding through the assistance of AI and with or without human intervention will significantly lower the operational cost and enhance coding quality, heralding the approach of an entirely autonomous, regulation-friendly, and AI-led future for the CAC software industry.
A Comparative Market Shift Analysis 2020 to 2024 vs. 2025 to 2035
| 2020 to 2024 | 2025 to 2035 |
|---|---|
| Adoption rose due to increasing medical coding complexity and regulatory needs. Focus on improving coding productivity and precision. | It is widely used across healthcare segments, with AI-driven solutions automating coding and ensuring compliance with evolving standards. |
| Compliance with ICD-10, CPT, and regulatory standards like HIPAA drove adoption. | More regulations and global healthcare standards require periodic updates in CAC algorithms and compliance procedures. |
| Early adoption of Electronic Health Records (EHR) systems, with a focus on NLP (Natural Language Processing). | Sophisticated AI, machine learning and deep learning improve coding accuracy, and cloud-based deployment achieves scalability and accessibility. |
| AI is applied in code suggestions and minimizes manual entry. | Complete automation of coding activities with AI-enabled real-time auditing and automated claim submission. |
| Limited interoperability with other healthcare IT systems. | Smooth integration with EHRs, practice management systems, and billing systems, building harmonious data environments. |
| Country | CAGR (2025 to 2035) |
|---|---|
| USA | 9.5% |
| UK | 9.9% |
| France | 8.5% |
| Germany | 8.7% |
| Italy | 8.3% |
| South Korea | 10.2% |
| Japan | 9.1% |
| China | 10.8% |
| Australia | 8.9% |
| New Zealand | 8.4% |
The USA has monopolized CAC software production because it has a complex healthcare system and stringent regulatory compliance. The prevalence and adoption of EHR, as well as AI-driven coding solutions, allow ease and accuracy in medical billing. Federal regulations, such as the use of ICD-10 and HIPAA regulations, fuel demand for coding automation. High-quality health IT companies, as well as ongoing investments in artificial intelligence (AI) and natural language processing (NLP), also fuel industry growth.
The UK CAC softwareindustry is growing steadily based on the National Health Service (NHS) 's efforts to digitalize healthcare. Increased use of AI-based coding systems will ease patient data processing and physician reimbursement. Government stimulus and upgradation of the healthcare IT infrastructure are promoting demand. Also, value-based care transition and a focus on minimizing administrative burden are some of the key drivers for market growth.
France's CAC software market is expanding as the country is trying to build digitized healthcare systems through its "Ma Santé 2022" initiative. Hospitals and private healthcare entities are implementing AI-powered coding solutions for improved medical billing, with an emphasis on interoperability and automation. Standard coding practices according to European standards ensure conformity and ease of revenue cycle management.
Well-established healthcare infrastructure in Germany and its strict regulatory environment drive high CAC software adoption. Electronic medical record adoption gained momentum with the adoption of the Digital Healthcare Act (DVG), driving demand for automated coding systems. The presence of top-ranked health tech companies, along with increasing investments in healthcare offerings supported by artificial intelligence, drives the growth rate of the market.
Italy is evolving as electronic health records (EHR) and hospital information systems gain ground, keeping a focus on maximizing coding effectiveness in medical processes. The digital healthcare-enabling government-initiated National Health Plan is moving towards billing automation in healthcare. Private health facilities are increasingly engaging with CAC solutions to maximize revenue cycles and avoid non-compliance with changing rules.
South Korea's CAC market is aggressive and growing robustly because of conducive government support for health innovation in digital format. Growth in AI-based health technology adoption, backed by the Korean Digital New Deal, has prompted more automation of coding among medical institutions, giving it a leading edge in the marketplace. Its high IT infrastructure and the extent of its smart hospital rollout also facilitate it.
Japan's increasing elderly population and expanding healthcare needs have propelled the need for effective medical coding systems. Government initiative for digitalization in the form of "Society 5.0" has motivated healthcare institutions to embrace AI-driven CAC solutions for medical billing automation and improving coding precision. NLP technology integrated into CAC software allows effortless management of the continually expanding load of patient data.
China's CAC software market is growing strongly, driven by gigantic-scale healthcare digitization programs under the "Healthy China 2030" initiative. The increased prevalence of chronic illness and hospitalizations requires effective coding systems. Government investment and utilization of AI in healthcare IT are driving demand for CAC solutions that improve coding accuracy and facilitate reimbursement processes.
Australia's CAC software industry is expanding with heightening interest in digitalization and healthcare interoperability. The adoption of electronic health record systems after the government's My Health Record initiative has also raised the demand for automated coding solutions. Hospitals and healthcare organizations are seeking AI-based CAC software as their first choice to increase operational efficiency and achieve accurate medical coding.
The New Zealand CAC software market is on the rise, with healthcare providers shifting towards electronic record-keeping and computer-based coding systems. Healthcare IT spending, including the National Health Information Platform, is enabling the utilization of AI-based CAC software. The growing demand for effective medical billing and revenue cycle management by hospitals is propelling the market.
| Solution | Share (2025) |
|---|---|
| Software | 65.3% |
By 2025, the Computer Assisted Coding (CAC) Software Market, with the Software segment (65.3%), is expected to hold the largest share due to the increasing adoption of artificial intelligence (AI) driven coding solutions in the healthcare sector. The Services segment (34.7%) is also critical to software implementation, training, and maintenance.
The software segment (65.3%) is showing growth because of a growing demand for automated coding solutions, which improve the accuracy and efficiency of medical billing. The leader in this space is 3M Health Information Systems, whose AI-powered CAC software has seen widespread adoption in North America and Europe.
Likewise, Optum360 provides strong NLP-based coding solutions for healthcare facilities in Asia-Pacific and Latin America. The need to comply with regulatory standards like ICD-10 and CPT coding further prompts hospitals and outpatient clinics to use software that integrates with electronic health records (EHR).
For CAC software to be implemented, maintained, and optimized seamlessly, the Services segment (34.7%) is indispensable. Nuance Communications offers extensive coding consultancy and support services in North America and Europe, enabling healthcare providers to improve revenue cycle management.
At the same time, Dolbey Systems said it has a growth area in providing training and technical support in the Middle East and Asia-Pacific, where hospitals are slowly adopting CAC technology. With increasing complexity in healthcare coding standards, the need for ongoing support services is paramount to ensure the software is utilized most efficiently, with the least number of errors, and is kept accurate with changing regulatory practices.
| Deployment | Share (2025) |
|---|---|
| Cloud-based | 54% |
The industry is expected to witness significant growth by 2025, and the cloud-based segment was observed to hold the largest share, accounting for 54% of the industry, owing to its scalability, ability to access data remotely, and cost-effectiveness. Likewise, the On-premise segment has a substantial share, predominantly among large healthcare organizations requiring enhanced data privacy and customized solutions, with a 26% share.
Cloud-based segment leads by accounting for a 54% share, as providers continue to shift to the cloud to be more streamlined and reduce IT infrastructure costs. AI-powered cloud CAC software from 3M Health Information Systems, the global leader that serves many of North America and Europe, updates codes in real-time to remain compliant Optum 360 has also perceived the increased demand for flexible and scalable healthcare IT systems in the Asia-Pacific region and has thus expanded its cloud-based CAC solutions.
Moreover, the cloud-based CAC software can be integrated quickly into electronic health records (EHR), which is why it is preferred by hospitals as well as outpatient clinics that are looking for automation and coding on a real-time basis.
On-premise segment (26%) Despite the increasing shift to cloud deployment, this segment is still relevant for healthcare facilities that value direct data control, security, and compliance. Nuance Communications provides powerful on-premise CAC solutions in North America and Europe to organizations bound by strict data privacy laws.
Dolbey Systems offers on-premise solutions in the Middle East and Asia-Pacific, where some hospitals in the region prefer to store data locally. Although cloud adoption is on the rise, on-premise CAC is still critical for institutions that require more control over their IT infrastructure.
There is rapid growth in the industry with the demand for effective medical coding, accurate billing, and compliance regulations. Thus, CAC is considered important for further automating medical coding with the probable guarantee of reducing human errors and shortening reimbursement cycles associated with coding practices as it becomes more popular with EHRs and value-based health models.
Additionally, by further embedding AI, NLP, and ML capabilities, their efficiency and accuracy are further refined and will become vital solutions for hospitals, outpatient facilities, and medical billing companies.
Companies such as 3M Health Information Systems, Optum (UnitedHealth Group), Nuance Communications (a Microsoft company), Cerner Corporation, and Dolbey Systems are the leading players. 3M and Optum lead relatively with AI-led CAC platforms that smoothly integrate with EHRs and clinical documentation systems and provide real-time coding suggestions and compliance checks.
Conversational AI and voice recognition from Nuance Communications, now part of Microsoft, add to reducing the administrative burden on healthcare professionals by enabling the company to streamline documentation and coding accuracy. Although it focuses on automated ICD-10 and CPT coding with embedded compliance tools, Cerner Corporation and Dolbey Systems offer flexible options in CAC solutions for large hospital networks and smaller medical practices.
Cloud applications, interoperability with EHRs, and advanced data analytics innovate CA software. Also, part of this trend is that companies are increasingly integrating predictive analytics and real-time auditing tools to improve coding quality and fraud detection in response to issues around claim denials and revenue cycle management. An additional new standardization of features is establishing AI-based speech-to-text technologies for clinicians to capture accurate documentation without any extra effort.
The competitive distinction is also governed through the applied regulations, but it further demands that the CAC solutions be in tandem with the ever-changing healthcare coding standards. These standards would include ICD-11, CPT, and HCPCS. Automated coding software that increases accuracy ensures regulatory adherence and diminishes the manual workload, which is gaining wide acceptance as healthcare providers look into their operations to enhance their efficiencies.
Cloud technology has quickly become CAC solutions by creating a lower entry barrier for new entrants. This has encouraged many mid-sized healthcare IT organizations and startups to develop a low-cost AI-powered coding solution targeted toward small to mid-sized healthcare organizations. There is high competition, requiring established players to leverage strategic partnerships, AI advancements, and acquisitions to maintain dominance.
Market Share Analysis by Company
| Company Name | Estimated Market Share (%) |
|---|---|
| 3M Health Information Systems | 25-30% |
| Optum (UnitedHealth Group) | 20-25% |
| Dolbey Systems, Inc. | 15-20% |
| Nuance Communications (Microsoft) | 10-15% |
| Cerner Corporation (Oracle Health) | 5-10% |
| Other Companies (combined) | 20-30% |
| Company Name | Key Offerings/Activities |
|---|---|
| 3M Health Information Systems | Offers 3M 360 Encompass, integrating CAC, clinical documentation improvement (CDI), and analytics into one platform. Focuses on NLP and AI-driven automation. |
| Optum (UnitedHealth Group) | Provides Optum CAC, emphasizing predictive analytics, compliance tracking, and coding accuracy for faster reimbursement. |
| Dolbey Systems, Inc. | Specializes in Fusion CAC, which enhances coding efficiency and integrates with various electronic health record (EHR) systems. |
| Nuance Communications (Microsoft) | Combines Dragon Medical One with CAC, leveraging speech recognition and AI to improve documentation accuracy. |
| Cerner Corporation (Oracle Health) | Offers seamless integration with Cerner’s EHR ecosystem, focusing on workflow optimization and real-time coding assistance. |
Key Company Insights
3M Health Information Systems (25-30%)
3M leads the industry with its flagship product, 3M 360 Encompass, which integrates CAC, CDI, and performance analytics.
Optum (UnitedHealth Group) (20-25%)
Optum focuses on predictive analytics and compliance tracking through its Optum CAC solution.
Dolbey Systems, Inc. (15-20%)
Dolbey’sFusion CAC platform emphasizes efficiency and flexibility, making it popular among mid-sized healthcare providers.
Nuance Communications (Microsoft) (10-15%)
Since Microsoft acquired Nuance, the company has integrated its Dragon Medical One speech recognition technology with CAC solutions.
Cerner Corporation (Oracle Health) (5-10%)
Cerner’s CAC solutions focus on seamless integration with its proprietary EHR ecosystem.
Other Key Players (20-30% Combined)
The market is expected to reach USD 6.5 billion in 2025.
The market is projected to grow to USD 15.8 billion by 2035.
China is expected to experience the highest growth, with a CAGR of 10.8% during the forecast period.
The Cloud-based segment is one of the most widely adopted categories in the market.
Leading companies include 3M Health Information Systems, Optum (UnitedHealth Group), Dolbey Systems, Inc., Nuance Communications (Microsoft), Cerner Corporation (Oracle Health), Epic Systems Corporation, ZyDoc, Artificial Medical Intelligence (AMI), and Meditech.
The segmentation is into Software (Standalone CAC Software, Integrated CAC Software) and Services (Support & Maintenance Services, Education & Training Services).
The segmentation isinto cloud-based, on-premise, and web-based.
The segmentation isinto Clinical Code Auditing, Management Reporting & Analytics, Automated Computer-Assisted Encoding, and Others.
The report covers North America, Latin America, Europe, East Asia, South Asia & Pacific, and the Middle East & Africa.
DC Power Systems Market Trends - Growth, Demand & Forecast 2025 to 2035
Residential VoIP Services Market Insights – Trends & Forecast 2025 to 2035
Switching Mode Power Supply Market - Growth & Forecast 2025 to 2035
Safety Mirrors Market - Growth & Forecast 2025 to 2035
Heat Interface Unit Market Analysis - Size, Demand & Forecast 2025 to 2035
Induction Motors Market - Growth & Demand 2025 to 2035
Thank you!
You will receive an email from our Business Development Manager. Please be sure to check your SPAM/JUNK folder too.